Prognostication Post Arrest
Short Notes
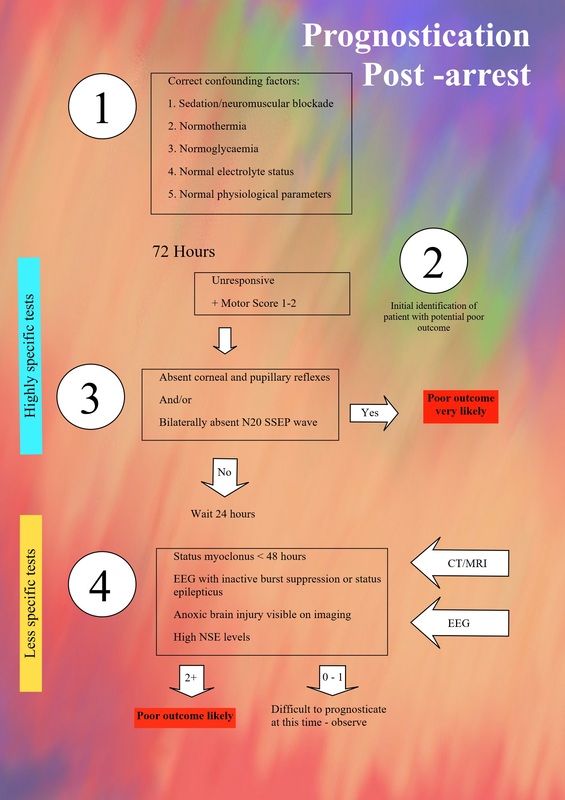
Prognostication cannot be determined before 72 hours.
The process involves the gathering of information with the greatest specificity as possible to minimise false positive rates.
If not meeting these criteria, prognostication will be more challenging and require further observation and assessment.
The process involves the gathering of information with the greatest specificity as possible to minimise false positive rates.
- Ensure no confounding factors:
- Allow time for metabolism of sedation/neuromuscular blockade (allow at least 12 hours)
- Normothermia
- Normoglycaemia
- Normal electrolyte status
- Normal physiological parameters (BP, CO2)
- Assess at 72 hours post arrest to identify patients with a potential poor prognosis – Still unconscious with a GCS motor score of 1 or 2 (no response or extensor response to pain)
- Perform the most specific tests for poor outcome first, looking for:
- Absent corneal and pupillary reflexes
- Bilaterally absent N20 SSEP wave
- If not prognostic, wait 24 hours before further assessment.
- Reassess to look for less specific tests:
- Status myoclonus < 48 hours after arrest
- EEG with unreactive burst suppression or status epilepticus
- Diffuse anoxic brain injury on imaging (CT or MRI)
- High NSE levels (marker of neuronal death)
If not meeting these criteria, prognostication will be more challenging and require further observation and assessment.
Long Notes
Prognostication is a very important part of post-cardiac arrest management. This is because of the high potential for significant neurological morbidity in these patients, and therefore the importance of being able to make decisions based on the best interests of these patients.
Prognostication should not be undertaken before 72 hours after the arrest, though the gathering of information can take place before this.
It is also important that medications are not affecting the assessment, particularly sedatives of neuromuscular blocking agents.
Prognostication should not be undertaken before 72 hours after the arrest, though the gathering of information can take place before this.
It is also important that medications are not affecting the assessment, particularly sedatives of neuromuscular blocking agents.
Tests should ideally have 100% specificity and a good sensitivity because of the significant implications.
There is also a potential for clinicians to be impacted by biasing factors from their own experience rather than a collection of objective information.
What is defined as a ‘meaningful’ or ‘good’ outcome is obviously open to some subjectivity, but there are some well-defined criteria to help.
The Cerebral Performance Category (CPC) is one such tool that is commonly used.
This is a 5 point scale describing degree of neurological disability:
The Modified Rankin Score is an alternative scoring system with a similar ranked system of worsening severity.
There is also a potential for clinicians to be impacted by biasing factors from their own experience rather than a collection of objective information.
What is defined as a ‘meaningful’ or ‘good’ outcome is obviously open to some subjectivity, but there are some well-defined criteria to help.
The Cerebral Performance Category (CPC) is one such tool that is commonly used.
This is a 5 point scale describing degree of neurological disability:
- Mild - no or mild psychological and neurological deficits. Able to work and live a normal life.
- Moderate – some disability but able to live with minimal support with daily life e.g. sheltered accommodation.
- Severe – conscious but dependent on others for care needs. Has at least limited cognition.
- Persistent vegetative state – Unconscious. Unaware of surroundings
- Death – Through conventional or brainstem death criteria
The Modified Rankin Score is an alternative scoring system with a similar ranked system of worsening severity.
The tests can be broken down into a number of categories.
Clinical Examination
Absent bilateral pupil reflexes at 72 hours has a false positive rate (FPR) of close to 0%, though it has a sensitivity of around 20%.
Bilateral absent corneal reflex has a similar prognostic power for a poor outcome.
An absent or extensor response to pain has a good sensitivity (around 75%) but a high FPR of about 27%.
Myoclonus refers to sudden, brief, intermittent jerks. A prolonged period of this is referred to as status myoclonus, generally if persisting over 30 minutes.
Myoclonic jerks are not consistently associated with poor outcome (FPR 9%).
However, Status Myoclonus starting within 48 hours of ROSC is strongly (though not universally) associated with a poor outcome (FPR 0%, 95% CI 0-5%), though with a poor sensitivity of 8 – 16%.
Evaluation of myoclonus should be done off sedation and with corroborating EEG to identify signs of awareness or reveal a coexistent epileptiform activity.
Bilateral absent corneal reflex has a similar prognostic power for a poor outcome.
An absent or extensor response to pain has a good sensitivity (around 75%) but a high FPR of about 27%.
Myoclonus refers to sudden, brief, intermittent jerks. A prolonged period of this is referred to as status myoclonus, generally if persisting over 30 minutes.
Myoclonic jerks are not consistently associated with poor outcome (FPR 9%).
However, Status Myoclonus starting within 48 hours of ROSC is strongly (though not universally) associated with a poor outcome (FPR 0%, 95% CI 0-5%), though with a poor sensitivity of 8 – 16%.
Evaluation of myoclonus should be done off sedation and with corroborating EEG to identify signs of awareness or reveal a coexistent epileptiform activity.
Electrophysiology
Short-latency Somatosensory Evoked Potentials (SSEPs) refers to the monitoring of the central response to a peripheral trigger, commonly the median nerve.
Bilateral loss of the N20 SEPP wave (a specific part of the response profile), strongly predicts death or vegetative state (FPR 0 – 2%, upper 95% CI 4%).
The majority of false positives appear to be artefactual, and indeed performing SSEPs requires specific skills and care
Electroencephalography (EEG) is another route for prognostication but is also helpful to provide other assessment.
This includes detecting non-convulsive seizure (which occur in about 25% of post-arrest patients) and assess level of consciousness which may be masked by a number of factors.
Absence of EEG reactivity (to stimuli like noise or tracheal suction) predicts a poor outcome, with a FPR of 0 – 2% (upper 95% CI 7%).
However, the definition of ‘lack of reactivity’ isn’t well standardised with a degree of inter-assessor variability.
Status epilepticus in patients managed with targeted temperature management is strongly related with a poor outcome, with a FPR of 0 – 6%. This is especially the case if there is an unreactive background.
Burst suppression is defined as more than 50% of the EEG recording with periods of voltage below 10 microvolts, with alternating bursts.
Though there has been some variation in this definition in the prognostication literature, persisting burst suppression beyond 72 hours is consistently associated with a poor outcome.
Bilateral loss of the N20 SEPP wave (a specific part of the response profile), strongly predicts death or vegetative state (FPR 0 – 2%, upper 95% CI 4%).
The majority of false positives appear to be artefactual, and indeed performing SSEPs requires specific skills and care
Electroencephalography (EEG) is another route for prognostication but is also helpful to provide other assessment.
This includes detecting non-convulsive seizure (which occur in about 25% of post-arrest patients) and assess level of consciousness which may be masked by a number of factors.
Absence of EEG reactivity (to stimuli like noise or tracheal suction) predicts a poor outcome, with a FPR of 0 – 2% (upper 95% CI 7%).
However, the definition of ‘lack of reactivity’ isn’t well standardised with a degree of inter-assessor variability.
Status epilepticus in patients managed with targeted temperature management is strongly related with a poor outcome, with a FPR of 0 – 6%. This is especially the case if there is an unreactive background.
Burst suppression is defined as more than 50% of the EEG recording with periods of voltage below 10 microvolts, with alternating bursts.
Though there has been some variation in this definition in the prognostication literature, persisting burst suppression beyond 72 hours is consistently associated with a poor outcome.
Imaging
CT scanning can demonstrate radiographic changes of a global anoxic cerebral insult.
The main finding is cerebral oedema, demonstrated by sulcal effacement and loss of grey/white matter differentiation.
Magnetic resonance imaging (MRI) can provide greater sensitivity for detecting anoxic brain injury, but it can be more problematic to perform on clinically unstable patients.
The main finding is cerebral oedema, demonstrated by sulcal effacement and loss of grey/white matter differentiation.
Magnetic resonance imaging (MRI) can provide greater sensitivity for detecting anoxic brain injury, but it can be more problematic to perform on clinically unstable patients.
Biomarkers
There are some biomarkers that a released as part of the brain injury and so may have a role in identifying this injury (a bit like troponins). Neuron specific enolase (NSE) is an example of this.
Problems with them include setting a value that provides a 0% FPR, which is challenging on what is effectively a continuous scale.
There is also potential for variation between analysers and outside sources (e.g. haemolysis).
As such these markers aren’t yet recommended as part of a prognostication strategy.
Problems with them include setting a value that provides a 0% FPR, which is challenging on what is effectively a continuous scale.
There is also potential for variation between analysers and outside sources (e.g. haemolysis).
As such these markers aren’t yet recommended as part of a prognostication strategy.
Prognostication Strategy
Bringing these factors together into an effective prognostication strategy requires a careful systematic approach to minimise interference, including assessor bias.
The approach involves identifying any potential confounding factors e.g. persisting sedation, before assessing for the most robust criteria first.
If these are present, prognositication can be done using these.
However, if they are absent, the process can employ other tests.
The approach involves identifying any potential confounding factors e.g. persisting sedation, before assessing for the most robust criteria first.
If these are present, prognositication can be done using these.
However, if they are absent, the process can employ other tests.
This is well described by the Resuscitation Council (UK) algorithm.
- Start with clinical assessment at 72 hours post ROSC.
- Ensure no impeding factors are present:
- Hypothermia
- Hypoglycaemia
- Sedation
- Major electrolyte abnormalities e.g. Sodium
- Normal physiological parameters e.g. BP
- Patients who remain comatose with absent or extensor motor response (M = 1 or 2) can be further evaluated.
- Test ocular reflexes (pupillary and corneal)
- Conduct SSEPs
If both of these are suggestive of poor neurological outcome, prognostication can be done at this stage as a poor outcome is very likely.
If they aren’t present, employ other assessment methods which have wider CI of FPR.
Delay assessment of these for 24 hours after initial assessment and reconfirm poor motor response.
If they aren’t present, employ other assessment methods which have wider CI of FPR.
Delay assessment of these for 24 hours after initial assessment and reconfirm poor motor response.
- Assess for presence of status myoclonus before 48 hours after ROSC
- Conduct EEG to look for evidence of burst suppression or status epilepticus.
- Look for evidence of anoxic brain injury on CT/MRI scanning.
- Consider measurement of NSE levels
A combination of these factors is recommended to help with prognostication.
If there is uncertainty, prolonged observation is recommended as absence of clinical improvement over time supports a poor outcome.
If there is uncertainty, prolonged observation is recommended as absence of clinical improvement over time supports a poor outcome.
Author: Tom Heaton
Last Updated: 8th May 2016
Last Updated: 8th May 2016
References & Links
- Resuscitation Council (UK). Post-resuscitation care. (Accessed 1st May 2016. Available at https://www.resus.org.uk/resuscitation-guidelines/post-resuscitation-care/)
- C Sandroni et al. Prognostication in comatose survivors of cardiac arrest: An advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Intensive Care Medicine. 2014. 40: 1816 – 1831.
- Medscape. General overview of somatosensory evoked potentials. 2014. (Accessed 20th April 2016, Available at http://emedicine.medscape.com/article/1139906-overview#a1)
- K Ajam et al. The reliability of the cerebral performance category to classify neurological status amongst survivors of ventricular fibrillation arrest. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2011. 19:38. http://www.sjtrem.com/content/19/1/38
- C Nickson. Prognosis after cardiac arrest. Life in the Fast Lane. http://lifeinthefastlane.com/ccc/prognosis-after-cardiac-arrest/_