Fascia Iliaca Block
Introduction
The fascia iliaca block is a relatively simple block that can be used to help with analgesia for pain affecting the hip joint, thigh and femur.
It involves instilling a large volume of local anaesthetic into the potential space below the fascia iliaca (hence the name).
This will hopefully spread to block the main anterior nerves of the thigh - the femoral nerve, lateral cutaneous nerve of the thigh (LCNT), and (less reliably) the obturator nerve
It involves instilling a large volume of local anaesthetic into the potential space below the fascia iliaca (hence the name).
This will hopefully spread to block the main anterior nerves of the thigh - the femoral nerve, lateral cutaneous nerve of the thigh (LCNT), and (less reliably) the obturator nerve
Anatomy
There are 4 main nerves that supply the lower limb:
As a short review of what these nerves do:
Femoral
Source: Lumbar Plexus, Anterior rami of L2,3,4
Sensation: Anteromedial aspect of thigh - medial aspect of leg and foot via saphenous nerve (its terminal branch)
Motor: Knee extensors - quadriceps, sartorius
Sciatic
Source: Lumbosacral plexus, anterior rami of L4 - S3
Sensation: Posterior aspect of thigh. All leg except for domain of the saphenous nerve
Motor: All posterior compartment of thigh. All muscles below knee.
Obturator
Source: Anterior rami of L2,3,4
Sensation: Variable area of medial aspect of thigh
Motor: Hip adductors
LCNT
Source: L2,3
Sensation: Lateral aspect of thigh, as distal as the knee
Motor: None
The sciatic nerve is a nerve of the posterior thigh and isn’t involved in the fascia iliaca block.
The block’s mechanism of action is dependent on the anatomy of the fascia iliaca compartment, so a quick review of this anatomy should help with understanding.
The Fascia Iliaca
This is a fascial layer of the posterior abdomen and thigh.
It extends from the thoracic vertebra down to the thigh where it blends with the fascia lata.
It covers the iliopsoas muscles, lining the posterior abdomen and pelvis.
This covering extends into the thigh where it forms the floor of the femoral canal.
Above the inguinal ligament it covers the femoral, obturator and LCNT.
This continues below the ligament, with the exception that the LCNT pierces the fascia to pass anteriorly at the level of the ligament, close to the ASIS.
The femoral vessels run anterior to the fascia.
The fascia iliaca compartment refers to the potential space between the fascia iliaca and the iliopsoas muscles.
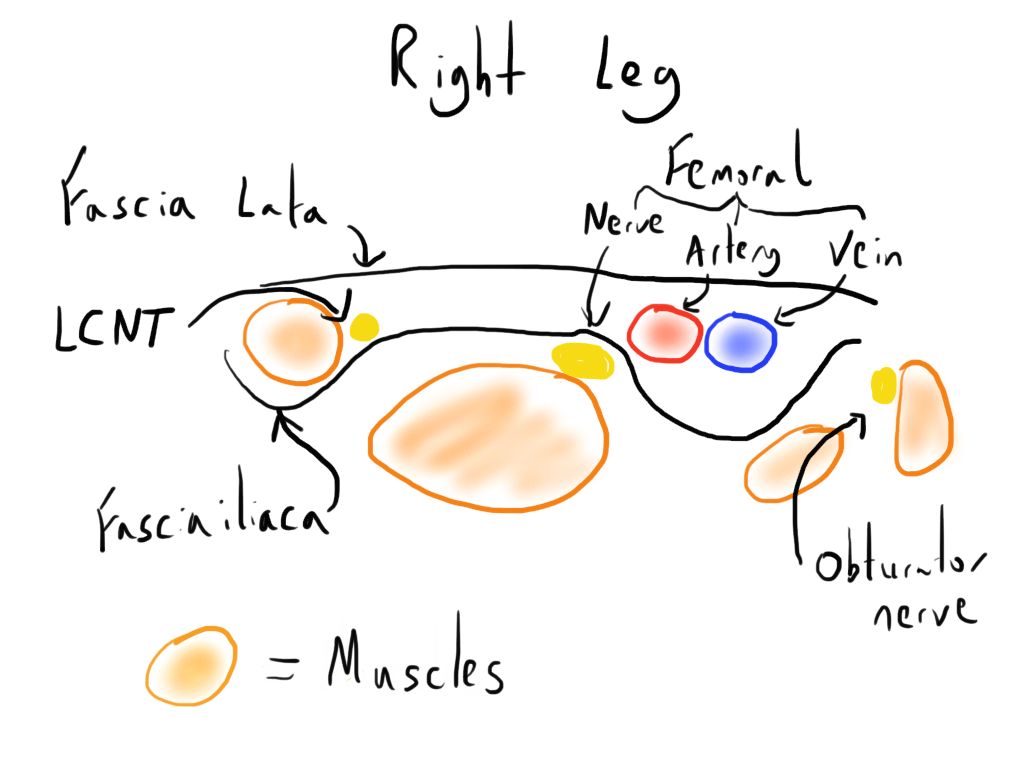
The image below is a cross section through the right leg just below the inguinal ligament - the lateral side is to the left and medial side to the right.
- Femoral
- Sciatic
- LCNT
- Obturator
As a short review of what these nerves do:
Femoral
Source: Lumbar Plexus, Anterior rami of L2,3,4
Sensation: Anteromedial aspect of thigh - medial aspect of leg and foot via saphenous nerve (its terminal branch)
Motor: Knee extensors - quadriceps, sartorius
Sciatic
Source: Lumbosacral plexus, anterior rami of L4 - S3
Sensation: Posterior aspect of thigh. All leg except for domain of the saphenous nerve
Motor: All posterior compartment of thigh. All muscles below knee.
Obturator
Source: Anterior rami of L2,3,4
Sensation: Variable area of medial aspect of thigh
Motor: Hip adductors
LCNT
Source: L2,3
Sensation: Lateral aspect of thigh, as distal as the knee
Motor: None
The sciatic nerve is a nerve of the posterior thigh and isn’t involved in the fascia iliaca block.
The block’s mechanism of action is dependent on the anatomy of the fascia iliaca compartment, so a quick review of this anatomy should help with understanding.
The Fascia Iliaca
This is a fascial layer of the posterior abdomen and thigh.
It extends from the thoracic vertebra down to the thigh where it blends with the fascia lata.
It covers the iliopsoas muscles, lining the posterior abdomen and pelvis.
This covering extends into the thigh where it forms the floor of the femoral canal.
Above the inguinal ligament it covers the femoral, obturator and LCNT.
This continues below the ligament, with the exception that the LCNT pierces the fascia to pass anteriorly at the level of the ligament, close to the ASIS.
The femoral vessels run anterior to the fascia.
The fascia iliaca compartment refers to the potential space between the fascia iliaca and the iliopsoas muscles.
The image below is a cross section through the right leg just below the inguinal ligament - the lateral side is to the left and medial side to the right.
The Fascia Iliaca Block
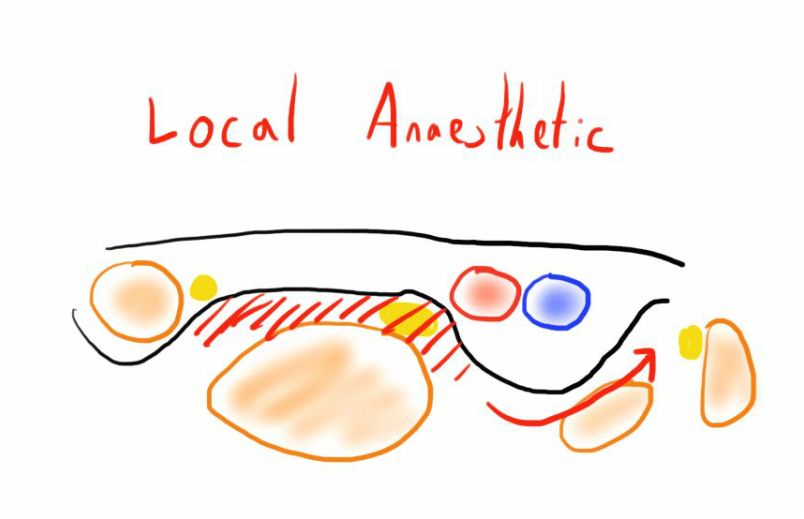
The block involves instilling a large volume of local anaesthetic into the fascia iliaca compartment.
Here the anaesthetic agent should block the femoral nerve and LCNT. There is also potential for the volume of anaesthetic agent to travel medially and block the obturator nerve, though this isn’t as reliable.
As noted above, this block doesn’t involve the sciatic nerve, whose innervation will remain intact.
The block can be performed with a landmark or ultrasound guided technique.
Unlike compared to other nerve blocks the landmark technique is not significantly worse than the ultrasound technique.
Uses/Indications
The nature of the block means it s not suitable for trying to achieve anaesthesia, but can provide good additional analgesia in some clinical cases:
Contraindications
The CI specific to the fascia iliaca block is previous femoral bypass surgery.
General block contraindications also factor e.g. infected site.
Local anaesthetic
1-2ml 1% Lidocaine for skin
30-40ml of local anaesthetic agent
e.g. 70 kg man, max safe dose bupivacaine is 140mg (2mg/kg)
Landmark technique
A blunt needle is best to use to get a good feel of the ‘pop’ with the fascia layers.
The landmark technique identifies the inguinal ligament initially.
Here the anaesthetic agent should block the femoral nerve and LCNT. There is also potential for the volume of anaesthetic agent to travel medially and block the obturator nerve, though this isn’t as reliable.
As noted above, this block doesn’t involve the sciatic nerve, whose innervation will remain intact.
The block can be performed with a landmark or ultrasound guided technique.
Unlike compared to other nerve blocks the landmark technique is not significantly worse than the ultrasound technique.
Uses/Indications
The nature of the block means it s not suitable for trying to achieve anaesthesia, but can provide good additional analgesia in some clinical cases:
- Analgesia for neck or shaft of femur fractures
- Analgesia for hip operations
- (When combined with a sciatic block) analgesia for knee and leg operations
Contraindications
The CI specific to the fascia iliaca block is previous femoral bypass surgery.
General block contraindications also factor e.g. infected site.
Local anaesthetic
1-2ml 1% Lidocaine for skin
30-40ml of local anaesthetic agent
- Long acting one makes more sense e.g. bupivacaine
- Concentration must be based on maximum safe dose for patient - this will often mean that the strengths used are fairly low.
e.g. 70 kg man, max safe dose bupivacaine is 140mg (2mg/kg)
- He could safely have 37ml of 0.375% bupivacaine
- Each ml of 0.375% is 3.75mg, therefore 140/3.75 = 37.333
Landmark technique
A blunt needle is best to use to get a good feel of the ‘pop’ with the fascia layers.
The landmark technique identifies the inguinal ligament initially.
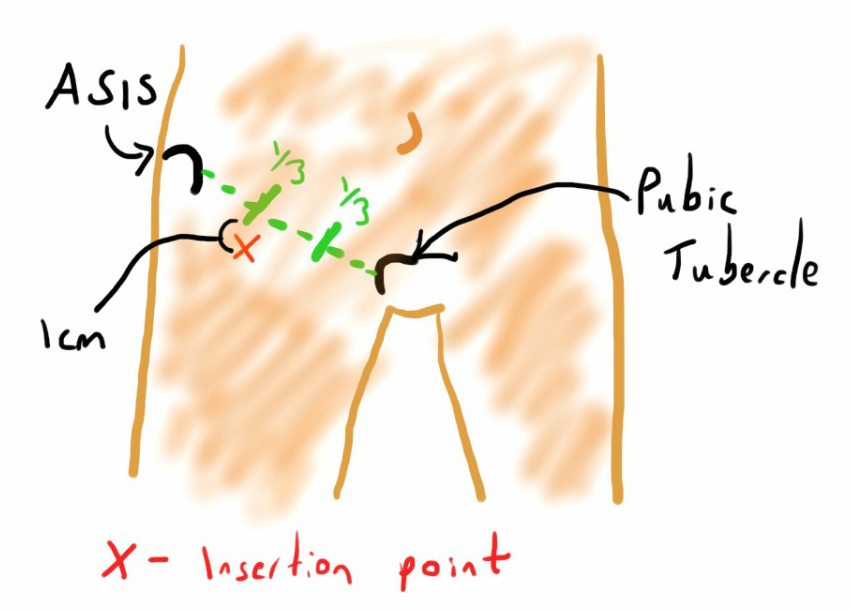
- A line is drawn between the anterior superior iliac spine (ASIS) and pubic tubercle.
- The line is divided into thirds.
- From the point between the lateral and middle third, go 1-2 cm inferiorly (towards the feet - this is the entry point
- Insert the needle through the skin
- Pass the needle down through the tissues, feeling 2 ‘pops’.
- Aspirate to ensure no blood before slow injection - should be low resistance.
Ultrasound guided technique
As with other US guided blocks, this involves identification of the correct plane, with visualisation of local anaesthetic spread there.
This depends initially on the identification of the anatomy as described above.
A couple of techniques are described.
The technique described by the New York School of Regional Anaesthesia involves imaging transversely at a level distal to the inguinal crease, similar to the site used in the landmark technique.
A depth of view of 3-5 cm using the linear transducer is optimal.
The technique involves:
As with other US guided blocks, this involves identification of the correct plane, with visualisation of local anaesthetic spread there.
This depends initially on the identification of the anatomy as described above.
A couple of techniques are described.
The technique described by the New York School of Regional Anaesthesia involves imaging transversely at a level distal to the inguinal crease, similar to the site used in the landmark technique.
A depth of view of 3-5 cm using the linear transducer is optimal.
The technique involves:
- Identification of the femoral artery.
- Identification of the fascia iliaca lateral to this.
- Insert the needle in laterally using an ‘in-plane’ approach.
- Visualise its passage through the fascia iliaca.
- The target location is about 3cm lateral to the femoral nerve
- The 2 pops of the landmark technique may be felt
- Observe spread of LA in the correct plane
- A small volume can be first instilled to confirm location
- Separation of the fascia from the ilacus muscle should be seen
- There should be medial and lateral spread
Image courtesy of NYSORA (Reference 3)
References
- AAGBI. Anaesthesia tutorial of the week. Accessed 18/01/2016. http://www.aagbi.org/sites/default/files/193-Fascia-Iliaca-compartment-block.pdf.
- Teachmeanatomy.info. Accessed 18/01/2016
- New York School of Regional Anaesthesia. Ultrasound guided fascia iliaca block. http://www.nysora.com/updates/3107-ultrasound-guided-fascia-iliaca-block.html