Cardiac Advanced Life Support
Cardiac arrest following cardiac surgery is often quite different from in other scenarios.
There are often different causes, and the degree of monitoring of the patient (they are often on the cardiac ICU), means that different approach is often warranted.
In particular, resternotomy and bypass play a role in the management of these patients.
The 2009 Clinical Guidelines Committee of the European Society of Cardiothoracic Surgery provides guidance on this different approach.
This approach is only recommended on the cardiac ICU, because of the nature of the time frame and equipment, although this may be varied depending on local protocol.
Main Differences
There are often different causes, and the degree of monitoring of the patient (they are often on the cardiac ICU), means that different approach is often warranted.
In particular, resternotomy and bypass play a role in the management of these patients.
The 2009 Clinical Guidelines Committee of the European Society of Cardiothoracic Surgery provides guidance on this different approach.
This approach is only recommended on the cardiac ICU, because of the nature of the time frame and equipment, although this may be varied depending on local protocol.
Main Differences
- In a shockable arrest rhythm (VF and pulseless VT), 3 attempts at DC cardioversion should be attempted before external chest compressions.
- In asystole or severe bradycardia, CPR can be withheld up to 1 minute to trial pacing.
- Routine adrenaline is not recommended as many causes of arrest can be quickly reversible and adrenaline may cause more complications.
A more detailed review of the management is now covered.
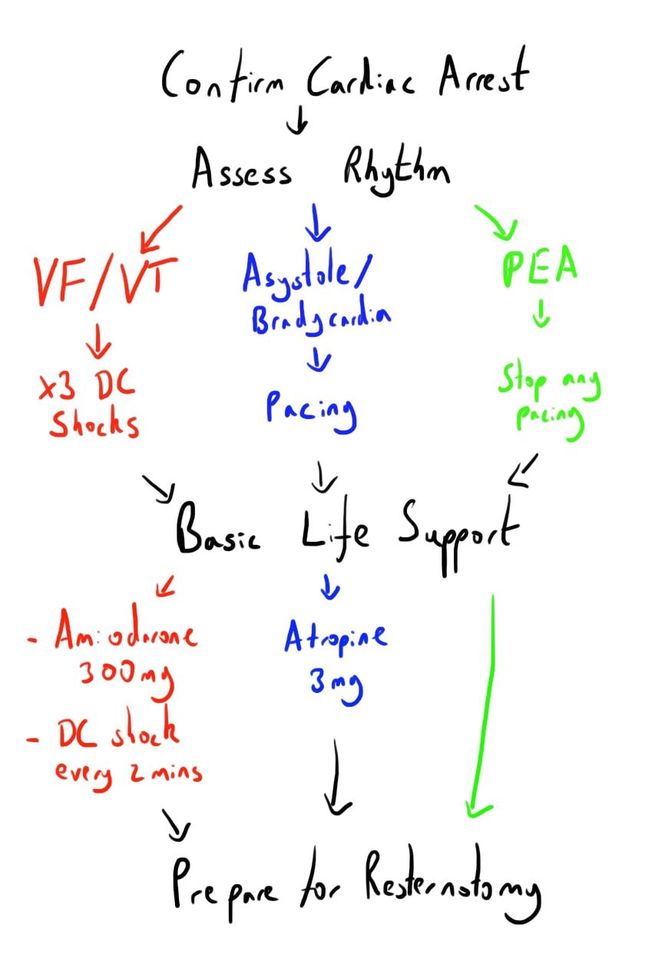
The image below provides an overview of the alternative algorithm.
The image below provides an overview of the alternative algorithm.
Initial Assessment
These patients will generally be on the cardiac ICU with high levels of monitoring (arterial line, CVC) and may be intubated and ventilated.
It is advised that these changes to ALS algorithms are limited to this environment.
Cardiac arrest will often be heralded by monitoring alarms e.g. ECG, arterial line.
If the ECG demonstrates a rhythm not compatible with cardiac output e.g. asystole, VF, then cardiac arrest should be called.
If the alarm is loss of arterial blood pressure, confirmation of cardiac arrest should be quickly established by assessing:
Once cardiac arrest has been confirmed, an emergency should be called.
It is advised that these changes to ALS algorithms are limited to this environment.
Cardiac arrest will often be heralded by monitoring alarms e.g. ECG, arterial line.
If the ECG demonstrates a rhythm not compatible with cardiac output e.g. asystole, VF, then cardiac arrest should be called.
If the alarm is loss of arterial blood pressure, confirmation of cardiac arrest should be quickly established by assessing:
- Central pulse
- CVP - waveform will be lost in cardiac arrest
- Capnography - will decrease and be lost in cardiac arrest
Once cardiac arrest has been confirmed, an emergency should be called.
Basic Life Support
This can be thought to consist of some key parts:
- External cardiac massage
- Airway and ventilation
- Drugs
External Cardiac Massage
The usual role of immediate external cardiac massage (ECM) is different in post cardiac surgery patients.
This is because:
Similarly, in asystole or profound bradycardia, a delay of maximum 1 minute in starting ECM is appropriate to trial pacing.
If this isn’t the case, chest compressions should be commenced as per normal ALS.
Adequacy of CPR should be guided by arterial waveform trace, aiming for a SBP of 60 mmHg.
If this is difficult, it may indicate a cause for the arrest that needs emergent resternotomy e.g. massive bleeding.
The usual role of immediate external cardiac massage (ECM) is different in post cardiac surgery patients.
This is because:
- Some rhythm disturbance causes of cardiac arrest e.g. VF can be rapidly corrected without a need for ECM.
- Chest compressions can cause trauma to the surgical site, risking further harm.
- Rapid detection of cardiac arrest in a highly monitored CICU environment means that there is a time window for intervention before ECM is needed.
Similarly, in asystole or profound bradycardia, a delay of maximum 1 minute in starting ECM is appropriate to trial pacing.
If this isn’t the case, chest compressions should be commenced as per normal ALS.
Adequacy of CPR should be guided by arterial waveform trace, aiming for a SBP of 60 mmHg.
If this is difficult, it may indicate a cause for the arrest that needs emergent resternotomy e.g. massive bleeding.
Airway and Ventilation
Patients may already be ventilated.
An airway/ventilatory problem is however an uncommon cause of cardiac arrest in this cohort.
However, initial management should involve:
Capnography also provides useful information.
If there is concern over OETT patency or location then it should be removed.
Consideration should be given to:
If the patient is not intubated then airway management should proceed as per ALS.
Patients may already be ventilated.
An airway/ventilatory problem is however an uncommon cause of cardiac arrest in this cohort.
However, initial management should involve:
- Increase FiO2 to 100%
- Confirm tube position and patency
- Confirm cuff inflation and no leak
- Confirm bilateral air entry
- Remove PEEP
Capnography also provides useful information.
If there is concern over OETT patency or location then it should be removed.
Consideration should be given to:
- Tension pneumothorax/heamothorax
- OETT migration
If the patient is not intubated then airway management should proceed as per ALS.
Drugs
Infusions
Patients may have drug infusions running.
These are more likely to be contributory to the arrest than helpful and should be stopped during cardiac arrest.
Adrenaline
Adrenaline is not recommended to be used routinely as in the ALS algorithms.
Part of this stems from the poor clinical evidence of any survival benefit from adrenaline.
Cardiac arrest following cardiac surgery is also more commonly from a rapidly reversible cause, which adrenaline does not help with and can indeed actually make worse e.g. bleeding.
It may be used by senior clinicians with a clear reason, and small, titrated doses may be useful in the peri-arrest phase.
Amiodarone
Amiodarone is the drug of choice for patients with a shockable refractory DC cardioversion.
It is recommended that 300mg is given as a bolus centrally if the 3 attempts at DC cardioversion fail.
A further bolus of 150mg can be consider if the arrhythmia remains refractory, before initiating the 900mg over 24h infusion.
Infusions
Patients may have drug infusions running.
These are more likely to be contributory to the arrest than helpful and should be stopped during cardiac arrest.
Adrenaline
Adrenaline is not recommended to be used routinely as in the ALS algorithms.
Part of this stems from the poor clinical evidence of any survival benefit from adrenaline.
Cardiac arrest following cardiac surgery is also more commonly from a rapidly reversible cause, which adrenaline does not help with and can indeed actually make worse e.g. bleeding.
It may be used by senior clinicians with a clear reason, and small, titrated doses may be useful in the peri-arrest phase.
Amiodarone
Amiodarone is the drug of choice for patients with a shockable refractory DC cardioversion.
It is recommended that 300mg is given as a bolus centrally if the 3 attempts at DC cardioversion fail.
A further bolus of 150mg can be consider if the arrhythmia remains refractory, before initiating the 900mg over 24h infusion.
Non Shockable Rhythm
Pacing
Pacing leads are often inserted at the end of cardiac surgery.
Some non shockable rhythm causes of cardiac arrest may be amenable to pacing to reverse the arrest - these are asystole and severe bradycardia.
Similar to shockable rhythms, an attempt at restoring cardiac output prior to chest compressions is recommended in these patients, providing that these attempts do not persist for greater than 1 minute.
In the case of patients with pacing leads in situ:
In the absence of pacing wires, external pacing via defibrillation pads can be used.
This process can take time to initiate (often more than 1 minute), so it is recommended that chest compressions are started.
If the cardiac arrest occurs during pacing, or the arrest rhythm is PEA with a pacing morphology, it is recommended to stop the pacemaker, in case it is masking underlying VF.
Pacing leads are often inserted at the end of cardiac surgery.
Some non shockable rhythm causes of cardiac arrest may be amenable to pacing to reverse the arrest - these are asystole and severe bradycardia.
Similar to shockable rhythms, an attempt at restoring cardiac output prior to chest compressions is recommended in these patients, providing that these attempts do not persist for greater than 1 minute.
In the case of patients with pacing leads in situ:
- Connect pacing lead to a pacemaker
- Set pacemaker to DDD at 90bpm
- Atrial and ventricular output should be set to maximum
In the absence of pacing wires, external pacing via defibrillation pads can be used.
This process can take time to initiate (often more than 1 minute), so it is recommended that chest compressions are started.
If the cardiac arrest occurs during pacing, or the arrest rhythm is PEA with a pacing morphology, it is recommended to stop the pacemaker, in case it is masking underlying VF.
Atropine
Unlike in ALS, the use of atropine is recommended in cases of asystole or bradycardia following cardiac surgery.
It is felt to be a low risk intervention which may reverse the cause of the arrest.
A bolus dose of 3mg is recommended.
Unlike in ALS, the use of atropine is recommended in cases of asystole or bradycardia following cardiac surgery.
It is felt to be a low risk intervention which may reverse the cause of the arrest.
A bolus dose of 3mg is recommended.
Resternotomy
Whilst a non shockable cardiac arrest rhythm in other scenarios is usually associated with a grim prognosis, the pathology is different following cardiac surgery and the prognosis is often very good.
The causes can include:
Basic hypoxic causes should have been corrected with BLS, whilst electrolyte disturbances are rare, and the prolonged time to correct will mean that open cardiac massage would be better.
As such, the priority is rapid resternotomy if the initial attempt at pacing and atropine fails to restore cardiac output.
Resternotomy will allow internal cardiac massage to be commenced.
This is associated with improved cardiovascular parameters compared with chest compressions (though mainly animal studies).
As such, any cardiac arrest following sternotomy which doesn’t respond to initial basic measures, should have a resternotomy.
Even if this may not provide a specific treatment, the benefits of internal cardiac massage would appear to justify it.
Resternotomy can therefore be beneficial for up to 10 days after cardiac surgery.
Whilst pathology that can be treated with sternotomy becomes less likely after the immediate postoperative period, the benefits of internal cardiac massage remain.
After 10 days though, there is increased chance of adhesions having formed, which complicates the procedure.
As such, resternotomy after this time must be made by an experienced clinician.
As noted, this approach to cardiac arrest is only really applicable on the cardiac ICU.
This is partly because of the factors involved in rapidity of detection and equipment, and the observed poorer outcomes from resternotomy if done in a ward environment.
It is also important that the cardiac arrest team work from the same protocol, and there is the risk of increasing heterogeneity outside of the CICU.
The causes can include:
- Tamponade (most common)
- Tension pneumothorax
- Haemorrhage with hypovolaemia
Basic hypoxic causes should have been corrected with BLS, whilst electrolyte disturbances are rare, and the prolonged time to correct will mean that open cardiac massage would be better.
As such, the priority is rapid resternotomy if the initial attempt at pacing and atropine fails to restore cardiac output.
Resternotomy will allow internal cardiac massage to be commenced.
This is associated with improved cardiovascular parameters compared with chest compressions (though mainly animal studies).
As such, any cardiac arrest following sternotomy which doesn’t respond to initial basic measures, should have a resternotomy.
Even if this may not provide a specific treatment, the benefits of internal cardiac massage would appear to justify it.
Resternotomy can therefore be beneficial for up to 10 days after cardiac surgery.
Whilst pathology that can be treated with sternotomy becomes less likely after the immediate postoperative period, the benefits of internal cardiac massage remain.
After 10 days though, there is increased chance of adhesions having formed, which complicates the procedure.
As such, resternotomy after this time must be made by an experienced clinician.
As noted, this approach to cardiac arrest is only really applicable on the cardiac ICU.
This is partly because of the factors involved in rapidity of detection and equipment, and the observed poorer outcomes from resternotomy if done in a ward environment.
It is also important that the cardiac arrest team work from the same protocol, and there is the risk of increasing heterogeneity outside of the CICU.
Resternotomy Procedure
The initial resternotomy should be able to be performed quickly to optimise outcome.
This will require suitable training and equipment.
A rapid resternotomy kit should be available on the ICU. This is smaller than a full kit for ease of use, containing:
- Thoracic drape
- Scalpel
- Wire clipper
- Heavy needle holder
- Single piece sternal retractor
Once cardiac arrest is called, 2-3 members of the team (usually including the surgeon) should immediately don sterile gown and gloves.
Hand washing is not recommended due to the significant time delay, as long as not touch application of gloves is done (i.e. using gown sleeves).
Although resternotomy may often not be needed, the time saved is valuable.
These team members will then prepare the kit for resternotomy whilst BLS and initial measures are employed.
The skin is not cleaned, as the time to allow for drying (which is where the cleaning action occurs) is unacceptable.
Instead the skin drape is used to cover the skin.
If the basic measure are unsuccessful, the resternotomy will go ahead.
The procedure will involve:
- Chest compression are stopped whilst wound dressing is removed and thoracic drape put on chest
- Scrubbed team member then takes over chest compressions
- When ready, the scalpel is used to cut down to the sternal wires
- Sternal wires are cut, and then removed with the heavy needle holder - this can be more effective as a 2 person effort.
- Once the wires are cut, the chest will open slightly, reducing tendion and possibly resolve the arrest.
- If not, the retractor should be deployed, and suction gently applied to any clot.
- If cardiac arrest is persisting, then there is the option for:
- Internal cardiac massage
- Internal defibrillation
Internal cardiac massage needs to be done carefully by someone experienced in it.
There is the risk of trauma to the heart, particularly to any grafts.
AN example video of resternotomy can be seen here:
https://www.youtube.com/watch?v=4ayjVNOPkFc
At the end of successful resternotomy, there will commonly be an antiseptic washout.
An additional dose of antibiotics may also be given to reduce the likelihood of infection
Cardiopulmonary bypass
This may be needed if the arrest is prolonged and not resolved by sternotomy and internal cardiac massage.
Heparinisation will be needed in this case, but the concern is that the circulation will clearly be very poor.
It is therefore recommended that 30,000 unit of heparin are given immediately at the decision for bypass, and a further 10,000 units be added to the reservoir.
The cannulae are inserted as normal, but may be held by an assistant until purse strings can be added.
This may be needed if the arrest is prolonged and not resolved by sternotomy and internal cardiac massage.
Heparinisation will be needed in this case, but the concern is that the circulation will clearly be very poor.
It is therefore recommended that 30,000 unit of heparin are given immediately at the decision for bypass, and a further 10,000 units be added to the reservoir.
The cannulae are inserted as normal, but may be held by an assistant until purse strings can be added.
Links & References
- Dunning, J. et al. Guideline for resuscitation in cardiac arrest after cardiac surgery. European journal of cardio-thoracic surgery. 2009. 36: 3-28.
- Nickson, C. Cardiac arrest management after cardiac surgery. LITFL. 2016. https://lifeinthefastlane.com/ccc/cardiac-arrest-management-after-cardiac-surgery/
- Melbourne Simulation. Resternotomy Simulation. 2014. Available at: https://www.youtube.com/watch?v=4ayjVNOPkFc